Anti-Reflux Surgery
Anti-reflux surgery is a treatment for acid reflux, also known as GORD (gastroesophageal reflux disease, also known as GERD in North America). GORD is a condition in which food or stomach acid comes back up from your stomach into the oesophagus. The oesophagus is the tube from your mouth to the stomach.
Typical symptoms of GORD include retrosternal/chest burning (heartburn), acid taste in the mouth often associated with hypersalivation (water brash), and nausea. Some people can wake in the night with choking caused by acid affecting their vocal cords. Others may notice acid or even a small amount of food will reflux back into their mouth when they bend down or lift something heavy (volume reflux).
What causes GORD?
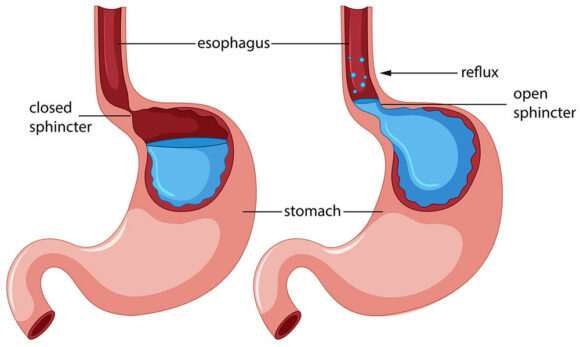
Reflux is usually caused by failure of the lower oesophageal sphincter – where the oesophagus meets the stomach. Most people will experience reflux during their lifetime though if the lower oesophageal sphincter does not close properly symptoms can be persistent and severe. A hiatus hernia can make GORD symptoms worse as it further weakens the body’s ability to control reflux. Severe GORD can occur in the absence of a hiatus hernia for reasons unknown. Many people find certain foods make reflux worse including spicy food, acidic food, caffeine, and alcohol. Smoking and being overweight can also make GORD worse.
Why have surgery for GORD?
Addressing dietary and lifestyle factors should be the first think you address though this typically only helps mild reflux. For most people anti-acid medications such as omeprazole and pantoprazole are very effective in the long-term control of GORD. People may choose surgery as an alternative though if they have side-effects from the medications, do not want to take the medicines long-term, or they are still getting major GORD symptoms despite being on a high dose of these medications. It is important to be certain that your symptoms are from GORD before considering this surgery, gastroscopy is routinely performed before making the decision and sometimes further tests such as 24hr acid studies and oesophageal manometry may be required.
Barrett’s Oesophagus is a pre-cancerous change in the lower oesophagus from long-term poorly controlled GORD. Good reflux control is essential in reducing the chance of this progressing to cancer. Medications and surgery are considered equally effective for this condition.
What is a hiatus hernia?
A hiatus hernia is when the stomach bulges through the oesophageal hiatus of the diaphragm. Typically it is only a small amount of stomach and it does not cause discomfort like groin and other abdominal wall hernias. It is a very common finding on gastroscopy and most people are not even aware they have a hiatus hernia. Treatment of small hiatus hernias is the treatment for GORD, either medications or anti-reflux surgery. Occasionally a hiatus hernia can be very large (most of the stomach has gone through the hiatus into the chest) in which case symptoms can be quite different and in which case surgery is advised to prevent major complications.
What are the anti-reflux operations?
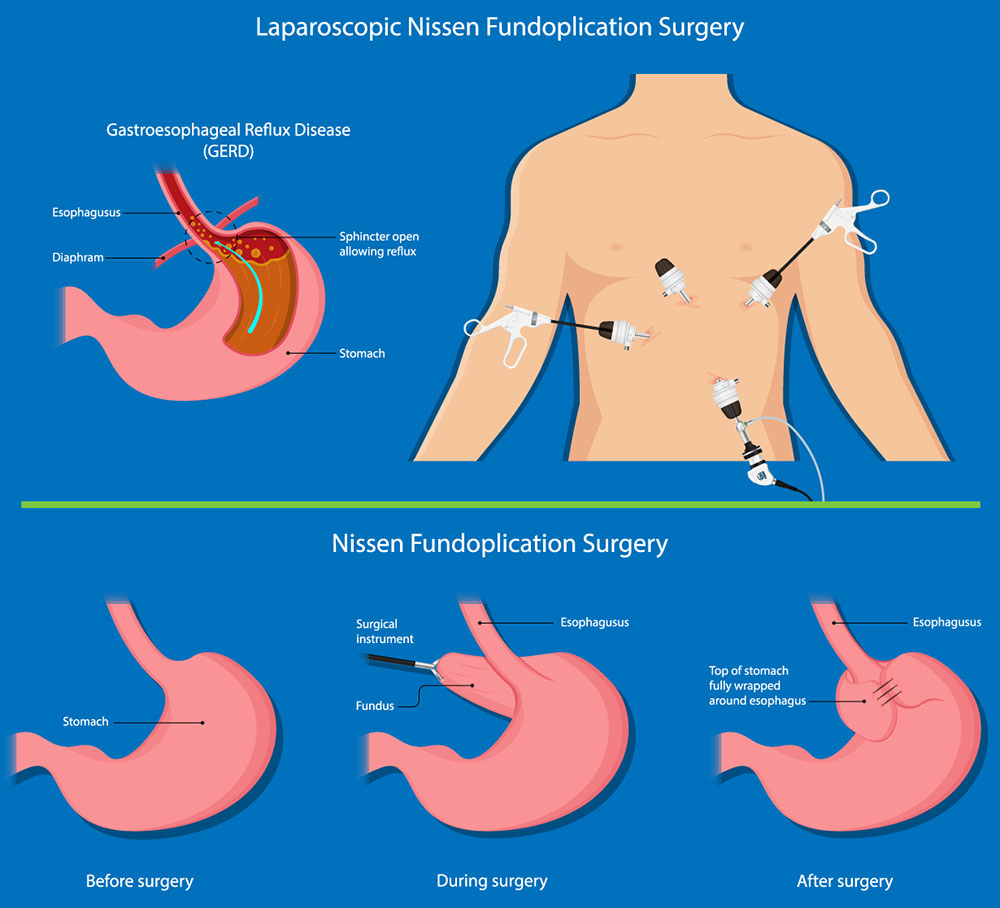
Modern anti-reflux surgery is almost always performed laparoscopic (keyhole). There are three main goals of surgery:
- Restore the lower oesophageal sphincter to the abdominal compartment
- Repair the hiatus hernia
- Perform a wrap of the stomach around the lower oesophagus to re-create/reinforce the sphincter (also called a fundoplication as the part of the stomach used is the fundus)
The main difference between the types of anti-reflux surgery is in how much of a wrap is formed, they all have names associated with the Surgeons who initially popularized them which can be confusing and stating the degree of wrap helps understand the differences better:
- Dor = anterior 90° wrap
- Watson = anterior 180° wrap
- Toupet = posterior 270° wrap
- Nissen = posterior 360° wrap
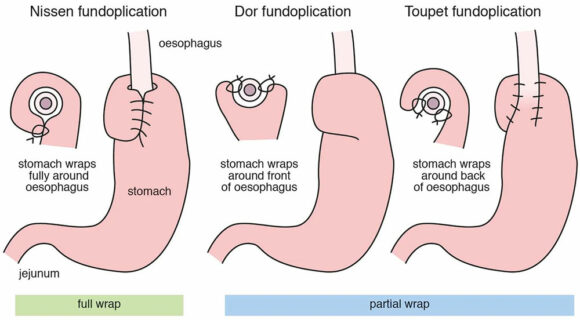
Picking the right wrap is a balance between reflux control and side effects as well as longevity. The best balance for most people has been shown to come from the posterior 270° degree wrap though there may be specific reasons in your situation making another wrap better for you. This should be discussed with your surgeon.
If you are significantly overweight (Body Mass Index (BMI) > 35 conventional anti-reflux surgery has a much higher rate of long-term failure and Roux-en-Y gastric bypass may be a better option for you – which has the added advantage of helping you lose much of your excess weight.
The usual surgery pathway
You will come into hospital on the day of your surgery. It is performed under a general anaesthetic (you are completely asleep). The operation typically takes 2 hours. After surgery you may require strong painkillers and anti-nausea medications, particularly within the first 24hrs though this rapidly improves. You can go home when you are comfortable enough and can drink enough which is usually after two nights in hospital, sometimes only after one night.
Following surgery, you will need to have a progressive diet as things are very tight to begin with. It is typically two weeks of liquids only, then two weeks of puree, then two weeks of soft food with commencement of normal food by 6-8 weeks. Some foods like rare steak, fresh bread, and lettuce leaves may take a few months before you can enjoy them.
Return to work is typically after two weeks for light activities but if your job involves strenuous activities you may need four weeks off. Recovery is also affected by your age and other health conditions. Recovery is typically slower for those aged over 65yrs and may be twice as long.
As with all major surgery, complications can occur though thankfully major complications are rare (1-2%). It is helpful to divide these into short-term complications that may occur during or shortly after surgery, and long-term complications which are more the side-effects of having had the surgery:
Short-term complications:
- Bleeding
- Injury to the spleen (it is attached to the upper part of the stomach, major injury may necessitate removing the spleen)
- Pneumothorax (air between the lung and chest wall, relatively common though only occasionally causes a problem, usually managed with a chest drain)
- Dysphagia (if the wrap or hiatus repair is too tight you may not be able to swallow anything and need to go back to surgery to have it loosened)
- Infection in the surgical fields/wounds
- Injury to the oesophagus or stomach
- Blood clots (DVT and PE)
Long term complications/side effects:
- Injury to the vagus nerve (Occurs at the time of surgery but is likely responsible for a lot of the long-term side effects listed that relate to gastric dysfunction)
- Gas bloat
- Early satiety (feel full with only a small meal)
- Increased flatulence
- Gastric dysmotility (symptoms can vary)
- Dysphagia – long-term (food getting stuck in the oesophagus)
- Recurrence of reflux and/or hiatus hernia
- Slipped wrap
- Weight loss (typically 10kg over the first few months)
The most important factor in determining outcomes is ensuring the operation is done for the right reasons. Over 90% of patients who undergo antireflux surgery have very good long term outcomes and report improved quality of life. Most people will come off all antacid medications; some may need to restart a low dose after a year or two though they still report better GORD control and better quality of life than before their surgery.
